基因檢測是診斷SMA很重要的工具
![1501169872024[1].png 1501169872024[1].png](/content/commercial-tw/specialty/sma/hcp/tw_tw/home/disease-education/sma-diagnosis/_jcr_content/mainpar/image_1076575629.img.png/1511854975585.png)
建議將SMN1基因缺失試驗作為疑似患有脊髓性肌肉萎縮症患者的第一診斷步驟。
可以經由聚合酶鍊式反應 (PCR) 測定來確定兩個染色體上的SMN1第七外顯子7是否缺失,此缺失在95%的SMA病患中發生。dPCR能夠可靠且準確地測量的SMN1和SMN2基因數量(即0-6個拷貝數)。5,9
使用微珠技術的分子 基因檢測證明:
高靈敏度(正確識別缺乏SMN1第七外顯子的血液樣本)
高特異性(正確識別SMA帶因者、正確識別不受影響的樣本)
如果發現患者具有單一SMN1基因但是臨床表現卻疑似患有SMA,應進行SMN1基因定序分析,以確定SMA的診斷。7
先天性低張力相關疾病基因檢測套組可用來測試脊髓性肌肉萎縮症。這類套組可以提供包括脊髓性肌肉萎縮、myotonic dystrophy(第1型)、Prader-Willi綜合症、Angelman症候群、maternal uniparental disomy 14(UPD 14)等疾病的檢驗。11-13
先天性低張力相關疾病基因檢測套組通常只包括SMN1基因的缺失試驗。可以根據需求安排SMN2拷貝數目的檢試。5,14
如果出現SMA症狀的病患,但卻有2個SMN1基因,那麼在鑑別診斷中可能會考慮其他運動神經元失調的情況。5
國健署指定之基因診斷醫療機構
一、遺傳性疾病檢查:
(一)經中央主管機關認定之新生兒先天性代謝異常疾病篩檢。
(二)經中央主管機關認定之新生兒先天性代謝異常疾病陽性個案之確認診斷。
(三)海洋性貧血檢查。
(四)血液細胞遺傳學檢驗。
(五)產前遺傳診斷,包括細胞遺傳學檢驗、基因檢驗、生化遺傳學或其他產前遺傳診斷之檢驗。
(六)流產組織或死產者之確認診斷。
(七)其他經中央主管機關認定之遺傳性疾病檢查。
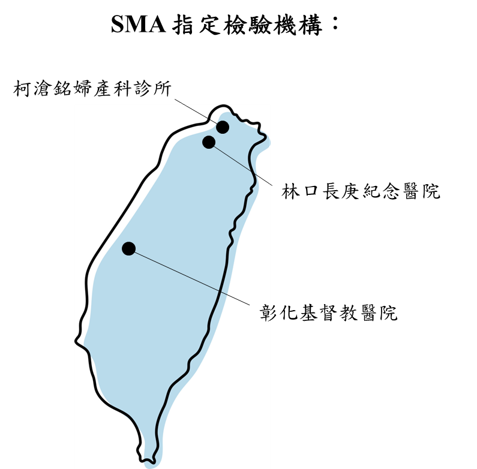
https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=4083&pid=411&sid=407
診斷延遲在SMA中很常見
一項系統性回顧研究,評估SMA延遲診斷的狀況。5篇關於發病年齡和確診年齡的報告顯示,SMA會延遲數個月到數年才能被正確診斷。16
SMA表現型 |
發病年齡(加權平均數, 標準差) |
確診年齡(加權平均數, 標準差) |
診斷延誤(加權平均數, 標準差) |
SMA表現型I型 |
發病年齡(加權平均數, 標準差)2.5個月(0.6) |
確診年齡(加權平均數, 標準差)6.3個月(2.2) |
Delay in diagnosis (weighted mean, SD)3.6個月 (1.9) |
SMA表現型II型 |
發病年齡(加權平均數, 標準差)8.3個月(1.6) |
確診年齡(加權平均數, 標準差)20.7個月(2.6) |
診斷延誤(加權平均數, 標準差)14.3個月 (0.0) |
SMA表現型III型 |
發病年齡(加權平均數, 標準差)39.0個月(32.6) |
確診年齡(加權平均數, 標準差)50.3個月(12.9) |
診斷延誤(加權平均數, 標準差)43.6個月(0.0) |
SD = 標準差
用來決定I型、II型、III型SMA的「加權平均診斷年齡」的研究數分別為4、4、3。16
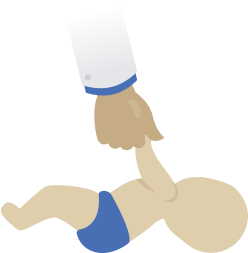
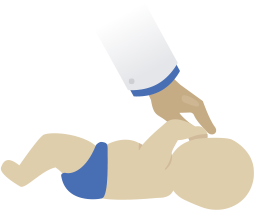
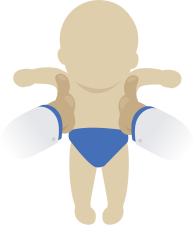
早期就被鑑定出患有SMA的新生兒也可以在症狀出現之前就開始接受治療。在以人類和老鼠為模型的研究中顯示早期治療對於疾病治療可能是最有效的。16
父母親在孩子被診斷出患有早發型與晚發型SMA之前皆描述曾有以下經驗17,18: |
||
|
關於脊髓性肌肉萎縮症更多的臨床資訊,請點擊這裡。
References
1. Lefebvre S, Bürglen L, Reboullet S, et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell. 1995;80(1):155-165.2. Kolb SJ, Kissel JT. Spinal muscular atrophy. Arch Neurol. 2011;68(8):979-984.3. Lunn MR, Wang CH. Spinal muscular atrophy. Lancet. 2008;371(9630):2120-2133.4. National Organization for Rare Diseases. Spinal muscular atrophy.5.Prior TW. Spinal muscular atrophy: newborn and carrier screening. Obstet Gynecol Clin N Am. 2010;37(1):23-36.6. Prior TW; Professional Practice Guidelines Committee. Carrier screening for spinal muscular atrophy. Genet Med. 2008;10(11):840-842.7.Wang CH, Finkel RS, Bertini ES, et al; and Participants of the International Conference on SMA Standard of Care. Consensus statement for standard of care in spinal muscular atrophy. J Child Neurol. 2007;22(8):1027-1049.8.D’Amico A, Mercuri E, Tiziano FD, Bertini E. Spinal muscular atrophy. Orphanet J Rare Dis.2011;6:71.9.Butchbach ME. Copy number variations in the survival motor neuron genes: implications for spinal muscular atrophy and other neurodegenerative diseases. Front Mol Biosci. 2016;3:7. 10.Pyatt RE, Mihal DC, Prior TW. Assessment of liquid microbead arrays for the screening of newborns for spinal muscular atrophy. Clin Chem. 2007;53(11):1879-1885.11.Allele Diagnostics. Congenital hypotonia panel: DMPK repeat analysis, methlyation 15q, SMN1, uniparental disomy 14. https://www.allelediagnostics.com/services/tests/19/congenital-hypotonia-panel/. Accessed March 15, 2017.12.EGL Genetics. Congenital hypotonia panel: spinal muscular atrophy deletions, Prader-Willi/Angelman syndrome methylation, myotonic dystrophy, and uniparental disomy 14. https://genetics.emory.edu/egl/tests/HY. Accessed March 15, 2017.13.Saint Francis Center for Genetic Testing. Newborn hypotonia panel (DM1, PWS and SMA). https://www.saintfrancis.com/genetics/pages/laboratory-services/molecular-genetics/available-molecular-genetics-tests/newborn-hypotonia-panel.aspx. Accessed March 15, 2017.14.NCBI. Congenital hypotonia panel. https://www.ncbi.nlm.nih.gov/gtr/tests/503277/. Updated June 15, 2016. Accessed March 15, 2017.15. Rothwell E, Anderson RA, Swoboda KJ, Stark L, Botkin JR. Public attitudes regarding a pilot study of newborn screening for spinal muscular atrophy. Am J Med Genet A. 2013;161A(4):679-686.16. Lin CS, Kalb SJ, Wei-Shi Y. Delay in diagnosis of spinal muscular atrophy: a systematic literature review. Pediatr Neurol. 2015;53:293-300.17. Qian Y, McGraw S, Henne J, Jarecki J, Hobby K, Yeh WS. Understanding the experiences and needs of individuals with Spinal Muscular Atrophy and their parents: a qualitative study. BMC Neurol. 2015;15:217. doi:10.1186/s12883-015-0473-3.18. Lawton SL, Hickerton C, Archibald AD, McClaren BJ, Metcalfe SA. A mixed methods exploration of families’ experiences of the diagnosis of childhood spinal muscular atrophy. Eur J Hum Genet. 2015;23(5):575-580.19. RTI International. RTI Center on newborn screening, ethics, and disability studies. https://www.rti.org/impact/strengthening-newborn-screening-programs. Accessed March 15, 2017.20. RTI to offer free genetic disease tests for North Carolina newborns. https://smanewstoday.com/2017/01/26/rti-international-to-offer-free-genetic-disease-testing-for-spinal-muscular-atrophy. Published January 26, 2017. Accessed March 15, 2017.21. Cure SMA. Cure SMA launches newborn screening coalition. http://www.curesma.org/news/cure-sma-launches-newborn.html. Published February 10, 2017. Accessed March 15, 2017.22. Leyenaar J, Camfield P, Camfield C. A schematic approach to hypotonia in infancy. Paediatr Child Health. 2005;10(7):397-400.23. Peredo DE, Hannibal MC. The floppy infant: evaluation of hypotonia. Pediatr Rev. 2009;30(9):e66-e76. 24. Gowda V, Parr J, Jayawant S. Evaluation of the floppy infant. Paediatr Child Health. 2007;18:1. 25. Bodensteiner JB. The evaluation of the hypotonic infant. Semin Pediatr Neurol. 2008;15(1):10-20.26. North KN. Clinical approach to the diagnosis of congenital myopathies. Semin Pediatr Neurol. 2011;18(4):216-220.27. Van Toorn R. Clinical approach to the floppy child. CME: Your SA Journal of CPD. 2004;22(8):449-455.28. McDonald CM. Clinical approach to the diagnostic evaluation of hereditary and acquired neuromuscular diseases. Phys Med Rehabil Clin N Am. 2012:23(3):495-563.29. Darras BT, Royden Jones H Jr, Ryan MM, De Vivo DC, eds. Neuromuscular Disorders of Infancy, Childhood, and Adolescence: A Clinician’s Approach. 2nd ed. London, UK: Elsevier; 2015. 30. Deenen JCW, Horlings CGC, Vershuuuren JJGM, et al. The epidemiology of neuromuscular disorders: a comprehensive overview of the literature. J Neuro Dis. 2015;73-85
診斷過程如何與父母/照護者的觀點不同?
了解更多